Menopause and Gut Health - how are they linked?
- Helen Ross
- Dec 11, 2022
- 4 min read
Updated: Dec 7, 2025

Menopause is a major life milestone for women, it is often associated with being a time of inner reflection and evaluation, and it marks a new phase of life.
The official diagnosis of menopause comes after 12 months has passed without a menstrual period, which usually occurs at around the average age of 51 years old. For a small number of women, it can occur earlier than that, sometimes in their early 40s, or even younger.
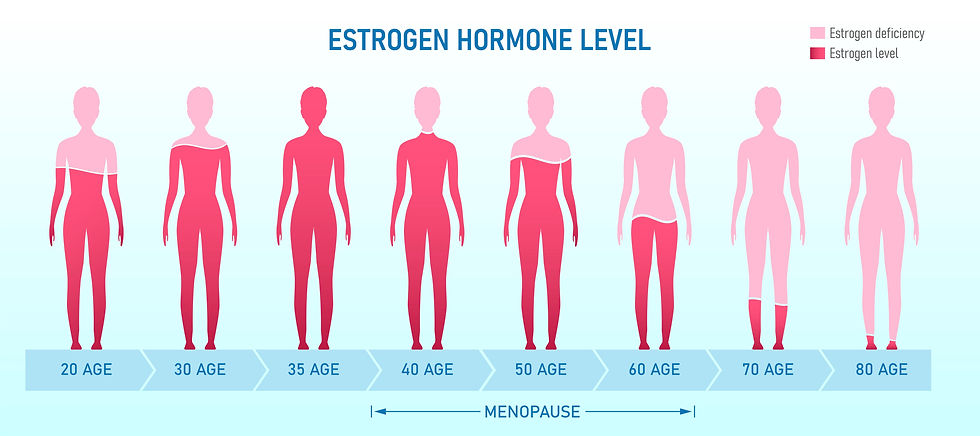
Declining levels of oestrogen, progesterone, and testosterone, mark the physiological changes that occur in the body. The ovaries stop producing oestrogen, but some oestrogen is still produced by the adrenal glands.
Common menopausal symptoms include hot flushes, mood changes (irritability, low mood, anxiety), night sweats and sleep disturbances, poor memory, weight gain (especially around the belly), vaginal dryness, low libido, and vaginal atrophy.
So how does our gut health impact our menopause?
One thing we know is that as we age, we need to pay greater attention to our nutrition and self-care. Addressing gut health and other health issues during peri-menopause can go a long way to preparing our bodies for a smoother menopause.
Women who have been prone to hormone issues during their menstruating years, may be more likely to have more impactful symptoms during menopause. Getting your gut health and hormones into balance as early as possible is a key strategy.
Some women go through a lot of emotional and physical distress during the menopause, while others sail through it, almost unnoticed.
Stress does seem to play a big role in the severity of symptoms.
Nutritional and lifestyle modifications, as well as ensuring optimal gut health can certainly make the transition a smoother ride.
Paying attention to our gut health is one of the cornerstones of overall health, especially as around 70% of our immune system lies within the gut, and many of our hormones are made in the gut.
Dysbiosis is a term used to describe an imbalance of gut bacteria, which is a common cause of irritable bowel syndrome (IBS). One way this imbalance can occur is after a course of antibiotics, when the good bacteria have been wiped out and the ‘opportunistic’ pathogens have overtaken the microbiota or microbiome (the trillions of bacteria that reside within the gut). Chronic stress, hormone changes, toxins, and other medications are all implicated in the onset of dysbiosis.
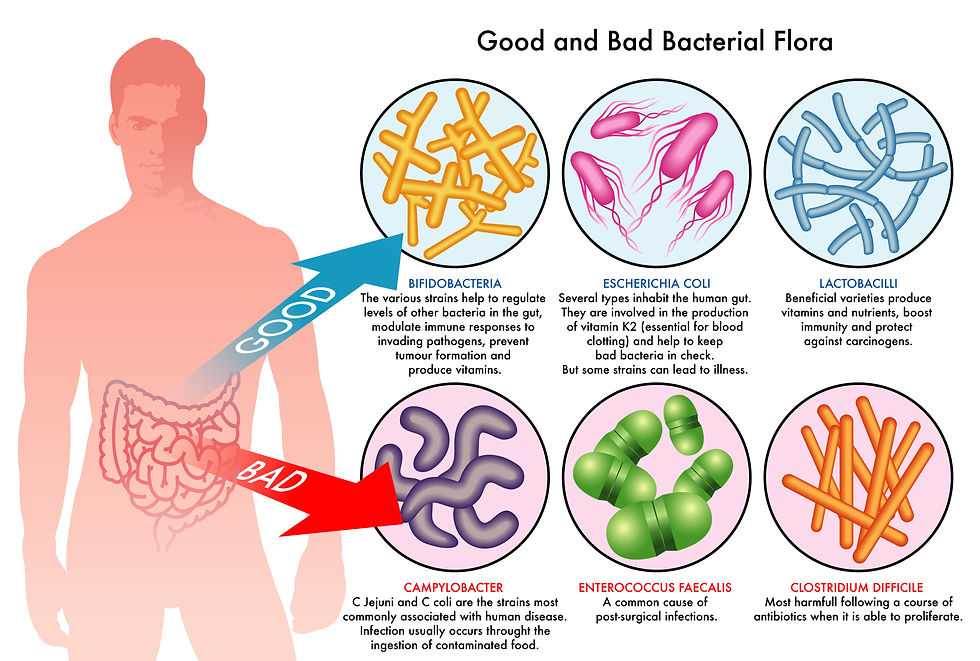
For women who have gone through the menopause, declining levels of oestrogen and progesterone, may also impact IBS symptoms. This is because declining hormone levels have a detrimental impact on our good gut bacteria.
Oestrogen protects the gut barrier and maintains the microbial diversity (e.g. healthy gut microbiome), therefore low oestrogen sets us up for a poor gut lining and potentially dysbiosis too.
Furthermore, oestrogen has anti-inflammatory effects in the gut, so when it declines, pro-inflammatory compounds can compromise the gut wall (or the gut lining) and promote an inflammatory cascade, which is also implicated in the onset of osteoporosis.
What can we do to support our gut health AND our hormones?
Firstly, if you have persistent IBS or digestive symptoms such as constipation, diarrhoea, bloating, or indigestion, it's recommended to get your gut back into balance. This is where microbiome stool testing comes in useful, as it helps us to pinpoint imbalances and work to correct them in a targeted way.
These are my top 3 tips for supporting your gut health and hormone balance:
1. EAT A RAINBOW

Eat a rainbow ~ eating a colourful, fibre-rich, nutrient-rich diet, increases antioxidants and phytonutrients.
It’s important to include a wide variety of vegetables, fruit, nuts, seeds, whole grains, legumes (lentils, beans, chickpeas), fresh herbs, spices, and herbal teas.
A diet high in processed foods is likely to exacerbate IBS and menopause symptoms, but there are also other key foods which can trigger your symptoms such as wheat or gluten, dairy, refined sugar, alcohol, and excessive caffeine.
2. INCLUDE FERMENTED FOODS

Including fermented foods in the diet helps to keep a healthy abundance of beneficial bacteria in the gut microbiome.
Fermented foods have been shown to:
Improve digestion, support healthy skin, improve mood – helps with anxiety and depression.
Also supports immunity and hormone balance, and increases metabolism and nutrient absorption.
* Please note that fermented foods are not great for everyone! For some people with gut imbalances, fermented foods can actually make their symptoms worse, and this will need to be assessed by an experienced practitioner.
Candida overgrowth, SIBO, or histamine intolerance can be a reason why you don’t tolerate these foods. Functional testing can help to identify these imbalances.
These conditions will always need to corrected before reintroducing probiotic-rich foods back into the diet.
3. MANAGE YOUR STRESS

When we are stressed, our body is in survival mode also known as ‘fight or flight’, which is triggered by the sympathetic nervous system, when our adrenal glands produce the stress hormones cortisol and adrenalin. Excessive cortisol can suppress our digestive function and tip the balance of our hormones. For optimal digestion, it is important that we are in a relaxed state, otherwise known as ‘rest and digest’, activated by the parasympathetic nervous system.
An increase in vagal tone from mindfulness-based stress reduction techniques such as yoga and meditation have been shown to reduce anxiety and depression, and therefore reducing the symptoms of IBS and menopause.
Need personalised help?
If you are struggling with your hormones or gut health, you may need personalised support to determine the cause and help you to regain balance. Functional laboratory testing and a thorough case history helps us to find the root cause of your issues.
Please get in touch if you’d like to learn more or book in a FREE 15-minute call to discover how to find relief from your symptoms.
The Microbiome Explorer is a microbiome stool test that looks at the health of the microbiome using metagenomic shotgun sequencing technology. It looks for pathogenic bacteria, fungal overgrowth, as well as parasites and commensal (beneficial) bacteria. It also assesses gastrointestinal health markers for inflammation, digestive enzyme function, and the integrity of the intestinal lining. Read more here.
The DUTCH Plus Hormones test measures sex and adrenal hormones along with their metabolites. Additionally, the daily (diurnal) pattern of free cortisol is included along with melatonin, and organic acid markers for B vitamins and neurotransmitters. Read more here.
Order your copy of The Simple Gut Reset Cookbook for some great gut-supporting recipes.







Comments